In recent months, the global health community has raised alarms about the resurgence of a potentially dangerous disease known as mpox, formerly called monkeypox. The World Health Organization (WHO) has declared a global health emergency in response to a surge in cases, particularly in regions previously not associated with the disease. But what exactly is mpox, where are these outbreaks occurring, and what steps is the WHO taking to address this growing crisis?
Understanding Mpox: Origins and Transmission
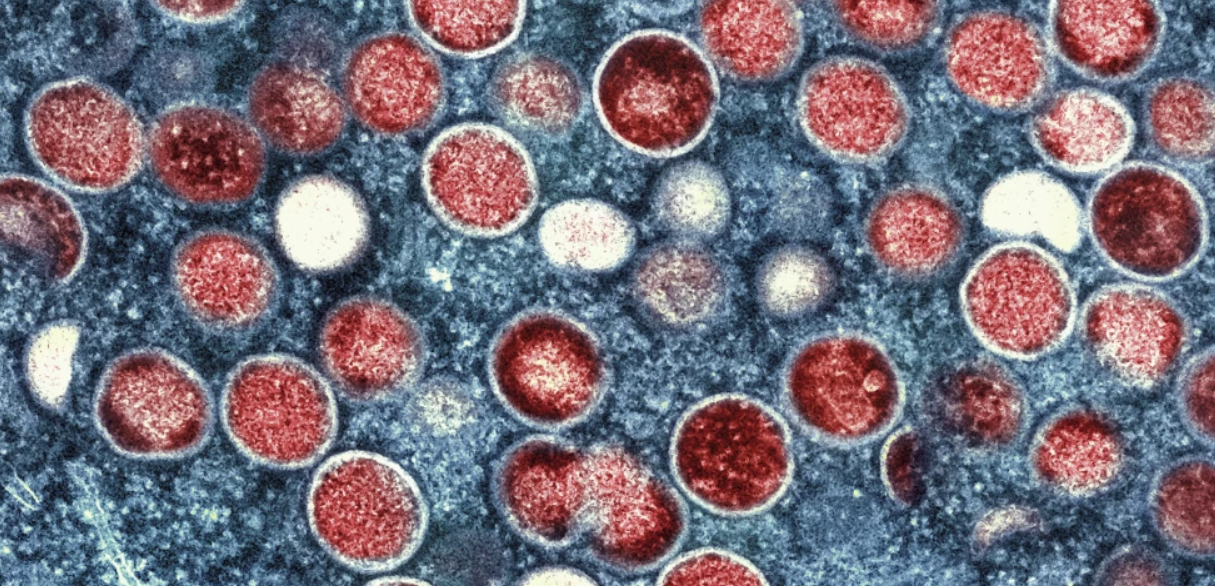
Mpox is a zoonotic viral disease caused by the monkeypox virus, which is part of the same family as the viruses causing smallpox and cowpox. First identified in 1958 among research monkeys, it was later found to circulate mainly among rodents and other small mammals in central and west Africa. The virus can be transmitted to humans through close contact with infected animals, but human-to-human transmission is more concerning in the current outbreaks.
The virus spreads primarily through direct contact with skin lesions, body fluids, or respiratory droplets from an infected person. It can also spread through contaminated objects, such as bedding or clothing. While not as easily transmissible as respiratory viruses like COVID-19, mpox’s long incubation period of up to three weeks and its often-mild early symptoms make early detection and containment challenging.
Symptoms and Health Risks
Mpox typically begins with flu-like symptoms, including fever, headache, muscle aches, and swollen lymph nodes, followed by a characteristic rash that starts on the face before spreading to other parts of the body. The rash progresses through several stages, from macules (flat, discolored patches) to vesicles (fluid-filled blisters), eventually forming scabs that fall off. While most cases are mild and resolve without specific treatment, severe cases can occur, particularly among children, pregnant individuals, and those with compromised immune systems. In rare cases, mpox can lead to complications like encephalitis, sepsis, and vision loss.
The Current Outbreaks: Regions Affected and Rising Concerns
Historically confined to Africa, mpox has seen a troubling spread in non-endemic countries since 2022. Initial clusters of cases emerged in Europe and North America, but as of mid-2024, outbreaks have been reported across multiple continents, including Asia, South America, and Oceania. The disease’s rapid spread in diverse settings—from urban centers to rural communities—has puzzled epidemiologists.
Countries like the United States, Brazil, Spain, and the United Kingdom have reported significant numbers of cases, with some regions declaring public health emergencies. Notably, the demographic profile of those affected has shifted. While the disease was historically linked to animal exposure in rural African regions, recent outbreaks have seen a rise in transmission among men who have sex with men (MSM) in high-density urban environments. However, experts caution against stigmatization, emphasizing that anyone can contract the virus through close contact.
WHO’s Response: Strategic Measures and Global Coordination
In response to the escalating outbreaks, the WHO has mobilized a comprehensive strategy to mitigate the spread of mpox. This strategy includes heightened surveillance, rapid response teams, targeted vaccination campaigns, and public awareness initiatives. The organization has classified mpox as a Public Health Emergency of International Concern (PHEIC), a designation that highlights the need for a coordinated international effort.
The WHO is working closely with governments, health agencies, and community organizations to promote vaccine distribution. Vaccines originally developed for smallpox, such as JYNNEOS and ACAM2000, have shown effectiveness against mpox. However, global supply remains limited, prompting the WHO to prioritize high-risk groups. The organization has also issued guidelines on case management, infection control, and preventive measures.
A significant aspect of the WHO’s response is countering misinformation and stigma. The organization has launched multilingual campaigns to educate the public about the nature of the virus, how it spreads, and the importance of early detection and care. Given the parallels to past health crises like HIV/AIDS and COVID-19, the WHO is urging a non-discriminatory, science-based approach to managing the outbreak.
Global Health Implications: Lessons and Future Directions
The mpox crisis underscores several important lessons for global health. Firstly, it highlights the interconnectedness of human, animal, and environmental health, a concept central to the One Health approach. Secondly, the spread of mpox beyond its traditional confines reflects broader challenges in global health equity, particularly the unequal distribution of resources and healthcare infrastructure. Lastly, the outbreak serves as a reminder that infectious diseases can emerge or re-emerge in unexpected ways, often influenced by factors like climate change, urbanization, and social behavior.
Looking forward, the WHO and other health authorities stress the need for sustained investment in global health systems. Strengthening early detection, ensuring rapid vaccine deployment, and fostering international collaboration will be crucial in preventing future pandemics. The mpox outbreak, while concerning, also presents an opportunity to refine global health strategies in an increasingly interconnected world.
Conclusion
Mpox’s emergence as a global health emergency is a stark reminder that the world remains vulnerable to infectious disease threats. As the WHO and its partners work to contain the virus and mitigate its impact, the situation demands both vigilance and compassion. By staying informed, promoting equity in healthcare access, and combating misinformation, societies can navigate this crisis and build resilience against future health emergencies.